Giving a voice to care home service users
Written by: Christine Jowsey - 17th December 2021
 Christine Jowsey is the Quality Improvement Manager at our Patient Safety Collaborative, which is delivered by the Improvement Academy as part of the Bradford Institute for Health Research. In this blog, Christine talks about the work that has been done to ensure care home residents are being given a say about how their care and support is delivered.
Christine Jowsey is the Quality Improvement Manager at our Patient Safety Collaborative, which is delivered by the Improvement Academy as part of the Bradford Institute for Health Research. In this blog, Christine talks about the work that has been done to ensure care home residents are being given a say about how their care and support is delivered.
The issues that are most important to service users will vary in every care home but asking the right questions and giving service users a voice may show that their priorities are not always what we think they might be. The service users’ voice can influence the staff in a way that mandated changes do not. It is a powerful voice and that’s why we’ve been working to improve the ‘Patient Measure of Safety’– a validated survey that is used in the hospital sector to ask patients for their observations and opinions.
During our initial work with our care home group, looking at the safety culture and asking staff to complete surveys, we were approached by service users asking to be involved. And why shouldn’t they? We ask patients their opinions in hospital, so why not care homes? This was our motivation for the creation of a new survey.
The previous tool needed alterations so that it was understandable and accessible for service users within the care sector, recognising that they have specific capabilities that needed to be taken into account during the design phase. We reviewed the tool to determine which questions from each of the domains were relevant whilst making sure the modifications didn’t negate the validity and purpose of the original survey.

Co-design partners
Through the review we reduced the number and complexity of the questions. Our co-design partners were a learning disability care home and we were pleased to be invited to join a focus group including care home staff and a service user. Within this group we co-designed the survey, discussing the wording and understanding with those who would be completing it. We also had access to a survey that the care home had produced themselves, which gave insight into the language that was accessible to service users. The discussions with the staff and service user representative helped us to recognise how many of the original questions might be misinterpreted and to consider new wording without altering the context.

An example of the survey
Key adaptations to the survey following the involvement of the service user representative included, changing the Likert icons as it became clear that the ones we had chosen caused confusion. We were advised by the service user that the icon faces needed to be distinct so that their meaning was clear. Something we had previously been unaware of was that service users recognise an icon showing “fingers to lips” as a symbol that they don’t want to answer a question, we therefore included this as an option for them to use when completing the survey. The service user also explained the value of their bedrooms, as this is their only personal space within a care home environment and helps them to feel safe and secure. With this in mind, we added a question about the service user bedrooms to the survey.
We followed the guidance of the group while making sure that we included all the domains, covering the principle objectives of the original questionnaire. Having redesigned the questions with the group, we then asked them to test it to see if the service users were able to understand and use it.
The care home issued the survey and had an 80% response rate and feedback was generally very positive. The service users were supported to complete the survey with the activity coordinators and some care staff. The survey was rolled out across the care home group and with sufficient data collected we then needed to ensure it met our original objectives and that it demonstrated validity. The Yorkshire Quality & Safety Research Group at Bradford Institute for Health Research performed a validity analysis on the survey and the results concluded that the 20 questions hung together reliably.
The survey analysis showed service users on the whole felt very safe in the care home and had their medicines as required. There were a couple of areas identified for improvement but the survey may be used to help service users focus on their own personal impact on others and thereby improve the experience for everyone.
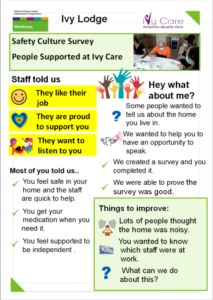
Poster summary of the results of the survey
We now have a tool that we can use for service user feedback in care homes as a measure of their perception of safety. As we move forward we will be able to survey both staff and residents concurrently to gain a clear view of the safety culture in individual homes. With joint feedback sessions and poster summaries of the results (appendix 2) we would hope to enable the development of shared improvement ideas from both staff and service users, helping teams to understand how culture is vital in creating, maintaining, and progressing a safe environment for care.
We would like to acknowledge the Ivy Care Group for their insightful input. Their ideas around the need for this tool, the manner in which to present it and the specific use of language were vital to its success. We would like to give special recognition to the guidance given by the service users without whom this story may never have materialised.
