Understanding how COVID-19 has changed our health and care system: impacts, innovations and learning
Posted: 23rd March 2021
 In this article our CEO Richard Stubbs reflects on the incredible work done in the past year to capture service transformations and lessons learnt across our region in response to the challenges posed by the pandemic.
In this article our CEO Richard Stubbs reflects on the incredible work done in the past year to capture service transformations and lessons learnt across our region in response to the challenges posed by the pandemic.
Exactly one year on from the beginning of the first lockdown, our health and care system is looking at a completely new world. Some of the changes first implemented as an immediate response to COVID-19 to protect patients and staff have permanently transformed the way health and care services will be delivered in the future. We have seen increased working with patients, families and carers to find work-arounds, embrace new technology and manage without their usual level of care or support, just to get through.
However, whilst the pandemic has brought about significant challenges and heartbreak for many, we have seen some excellent examples of resilience and triumph over adversity.
Over the past year, we have worked with colleagues from North East and Cumbria AHSN to complete a number of rapid insight reports (for each health and care system across the North East and Yorkshire region) to help get an idea of the impact of the pandemic so far on staff, patients and organisations.
The aim of these rapid insight reports and the case study overview was to summarise key learning and demonstrate the impact of the changes in the region, as well as possible risks, to share with our colleagues to inform future service planning in our area.
We have been privileged to hear from colleagues across the multiple organisations within each of the four integrated care systems across North East and Yorkshire including:
- West Yorkshire and Harrogate Health Care Partnership
- South Yorkshire and Bassetlaw Integrated Care System
- Humber, Coast and Vale Health and Care Partnership
- North East and North Cumbria Integrated Care System
Our work saw us receive over 470 responses to our rapid insights survey across the patch and undertake over 54 hours of dedicated interviews. We have produced over 30 dedicated case studies and supported 47 facilitated discussions and workshops to help generate our initial rapid insights reports for each system.
We have worked with clinicians, non-clinical staff, and patient representatives from a range of organisation including 76 patient representation groups.
Five factors that accelerated transformation
There was a vast amount of information collected from our partners across the region for consideration, but we found that changes to service could be grouped into several key areas (discussed in the section below), aided by what we found to be ‘key enablers for change’ – essential conditions that have allowed for the exceptional and rapid changes to have taken place:

- Funding – Funding has been made available to services during the pandemic to allow for the unparalleled blanket adoption of new technology, including software and equipment.
- Technology – This distribution and adoption of technology during the pandemic has been essential in the continuation of services by adapting the model of care to provide remote services and working patterns for staff where possible.
- Agility and attitude of the workforce – Praise has been given for the positive impact the staff themselves are having on the continuation of care across the region; specifically, their openness to change and willingness to adapt to new ways of working. This ‘can do’ attitude was echoed across the region and without it, new technologies and ways of working could not have been embedded as rapidly or efficiently.
- Collaboration – Overwhelmingly, at an individual as well as organisational level there has been a strong sense of ‘pulling together’ during the pandemic, which is allowing for ideas and information to be shared and processes to be embedded efficiently.
- Relaxation of bureaucracy – The quick changes to models of care, for example, have been made possible by the relaxing of regulations both at a wider national level and, we heard, at a managerial level within organisations themselves. This reduced bureaucracy has been widely welcomed amongst staff across the region and at all levels.
The areas most affected by change
We can group the changes resulting from the pandemic response as follows:
Remote working is here to stay
It will come as no surprise to learn that remote working was high on the agenda in the research feedback. Whilst there was an initial investment in the set-up (e.g. distribution of laptops and roll out of software), once established, remote working has led to minimum disruption to service in the face of national or local lockdowns and overall was received positively across the workforce. The majority of the feedback suggests that staff would like to continue to work from home at least some of the time post-pandemic. Overall, remote working has been found to improve a home/work balance by reducing travel time and maximising break times to spend with family and pets, having a positive impact on the health and wellbeing of staff.
Technology can improve patient experience and service efficiency
The rapid adoption of technology has also been mostly welcomed and praised by staff across the region – on balance, credited for saving both time and money. A multitude of new software has become commonplace since the start of the pandemic, most commonly Attend Anywhere, AccuRx and Microsoft Teams. This new software and technology has supported radical change, from efficient remote staff training and subsequent redeployment, to the rapid adaptation of patient pathways. Patient feedback has again, on the whole, been positive with regards to patient experience of this new technology, such as with remote consultations.
A joined-up workforce better equipped for future challenges
Undoubtedly it has been a time of great change for staff, who have responded with resilience, flexibility and overall positivity during this challenging time. Joined-up working at both an individual, team-level, as well as an organisation level, was a highlight from the research. There has been a willingness to share advice, expertise, skills and resources – a sense that everyone is working together towards one common goal. There have been numerous examples from across the region of teams offering to redeploy their staff to the frontline, and further of organisations working outside of their normal roles to meet service delivery. Virtual meetings have removed geographical barriers that might have prevented certain teams from meeting together regularly and the research points to an increased trust and understanding of partners as a result.
Patient safety still at the heart of decision-making
At the heart of all of the changes throughout the pandemic has been patient safety – the common direction that staff and services have been pulling towards together. Managing disruption to services by ensuring that treatments and appointments can continue as smoothly as possible has been the central catalyst for the amazing transformations we’ve seen across the service. Often, traditional care delivery pathways have been relaxed in order to prioritise patient safety, with changes such as the Discharge to Assess model in Humber Coast and Vale resulting in a reduction of hospital and care home admissions across the region. Our work found that staff have felt increasingly confident delivering remote care as the pandemic has progressed, improving telephone assessment skills and communication skills. Despite the amazing efforts we have seen, many patients and their families have not had access to the care they would have had under previously ‘normal’ circumstances. Waiting lists have grown and we need to ensure our continued focus on supporting access for patients going forward.
New post-pandemic leadership style emerging
Leaders have faced unchartered territory during this pandemic – how to manage huge service change and continuation of healthcare delivery, alongside supporting staff to manage personal changes and pressures. Ultimately, this has resulted in a new leadership style. Staff have sought visible, compassionate leadership as an antidote to the climate of fear and uncertainty. Virtual meetings have helped make senior leaders more accessible to staff, and regular check-ins have been appreciated by team members as the lines of communication between management and team members have remained open. We found that staff felt they have been more trusted and listened to, with senior staff more willing than ever to delegate tasks and grant autonomy for action. Overall, there was much hope from staff that this ‘new’ leadership style would continue post-pandemic.
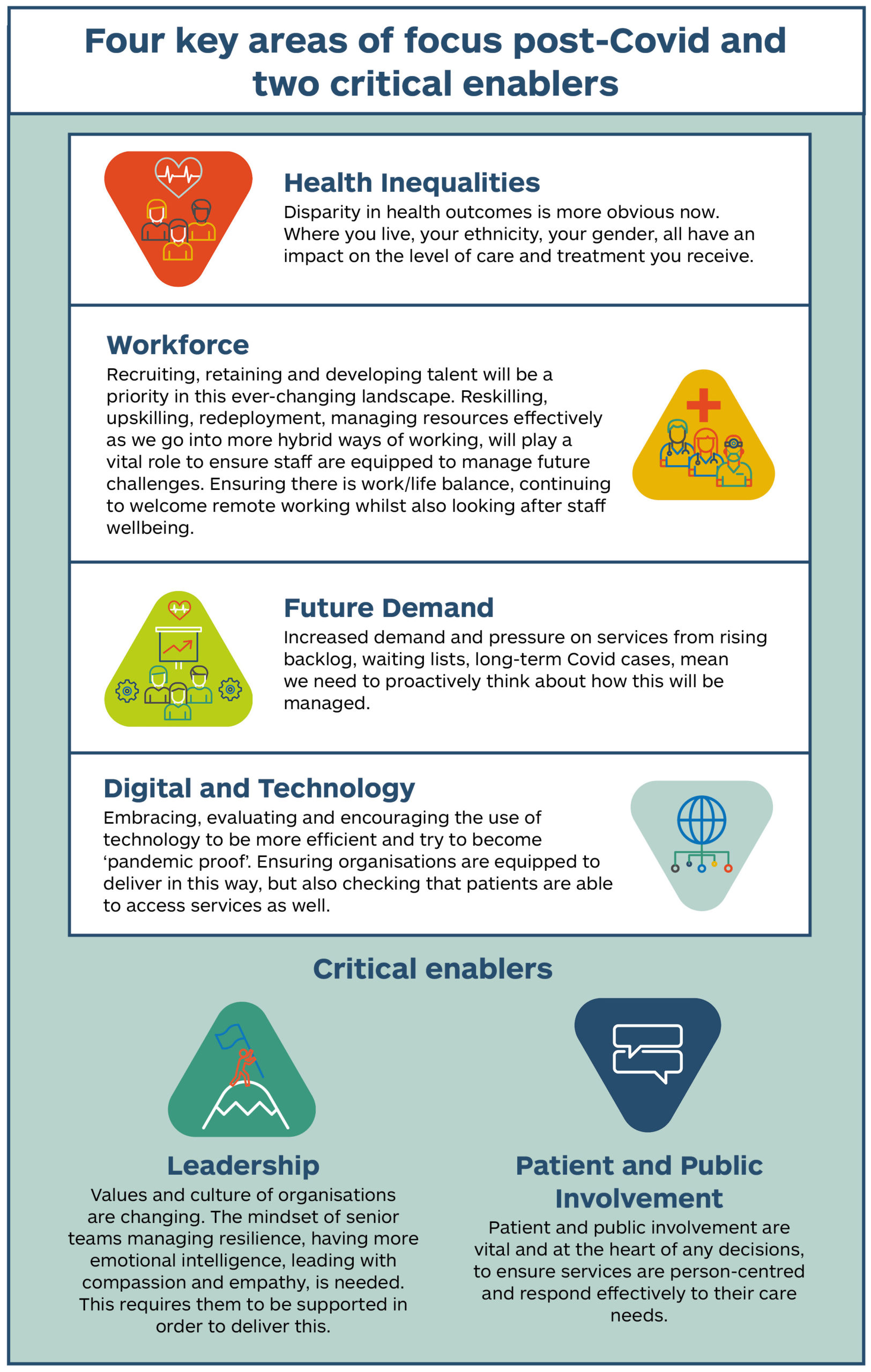
There is a risk that once the operational impact of the pandemic has diminished, we will see a tendency to return to previous ways of working. This is why it is essential for us to identify those innovations and behaviours that can help shape the services of the future and bring considerable benefits to the system as a whole.
We need to ensure that all the positive changes from the pandemic are retained. We know there is still work to be done looking at building the right infrastructures, funding models and staff support and training to facilitate the spread and adoption of innovations. Nevertheless, the pandemic has showed us how greater devolved leadership, collaboration with stakeholders, a mindset shift for both patients and clinicians who have now experienced a new way of delivering care, and local knowledge are all critical factors to succeed.
We want to continue to support and foster the enhanced partnership working across the North East and Yorkshire and help our health and care partners create a sustainable NHS for the future.
Find out about all the case studies developed across the region.
In this video, we hear from our partners and explore the implications of these significant changes across the North East and Yorkshire.
